Updated on July 5, 2024
You must have heard many times about appendicitis, which causes severe pain in the abdomen and is also a very dangerous disease in case of a ruptured appendix. In this article, find a review of appendicitis, appendicitis symptoms, causes, treatment, and nursing management. You can also watch her video teaching at the bottom. This article and video are mainly focused on the preparatory course for nurses who are planning to give their licensing exam for HAAD, MOH, DHA, Prometric, and NCLEX RN. But still, the contents are useful for general health information.
Review Of Appendicitis Symptoms Causes Management
The article is based on the below video teaching. You must watch the video at the bottom to understand well appendicitis symptoms, causes of appendicitis, treatment of appendicitis (appendectomy), and nursing management of a patient with appendicitis.
Review Of Appendicitis Symptoms Causes
What are appendicitis symptoms?
- What are the early warning signs of appendicitis?
- What is the main cause of appendicitis?
We are going to be talking about the review of appendicitis. Basically, appendicitis is a condition that is related to the gastrointestinal system. Before we start with what is appendicitis let’s take a look at what is appendix.
What is an appendix?

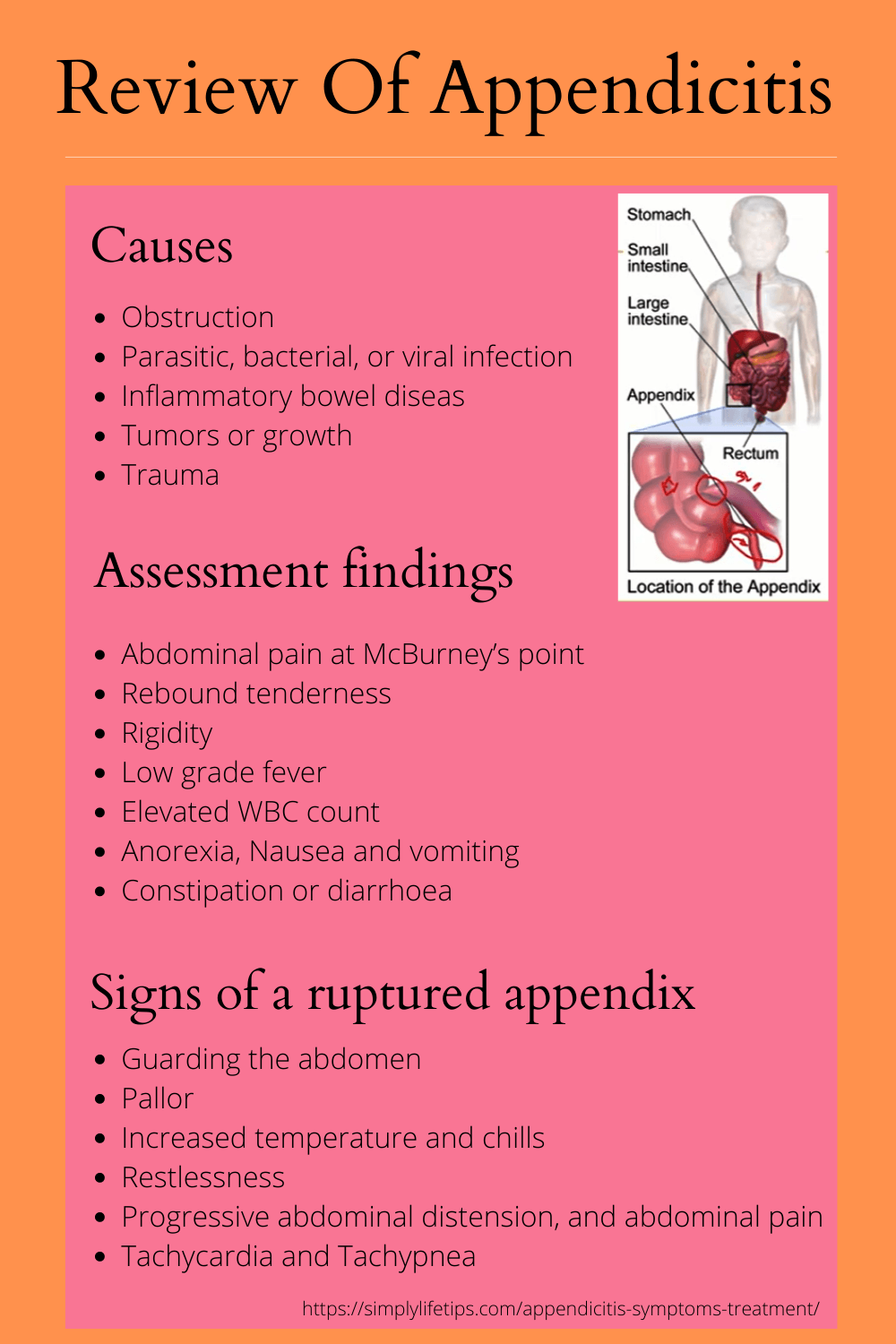
As you can see from the diagram, the appendix is part of the gastrointestinal system. So it’s basically a tube that connects to the large intestine end of it connecting to the large intestine at the point where the large intestine joins with the small intestine.
What is the function of the appendix?
If you want to talk about the function of the appendix there are different views. We do not completely know what is the function of the appendix. Some people believe that it has got a role to play in the immunity or basically it’s part of our immune system while others believe that it has got a role in the process of digestion but largely it is a vestigial organ.
Why appendix is called a vestigial organ?
What do we mean by a vestigial organ? A vestigial organ is an organ that has become redundant. And so probably at a time when evolution had not taken place, we had functioned for appendix with regards to digestion but revolution took place this particular organ does not have any role to play in the digestion or does not really help us with any of the digestive processes. And that’s how this organ has become redundant and that’s why we called as a vestigial organ.
So that is basically what is the function of the appendix. The appendix is also known as a vermiform appendix because it resembles a worm. If you look at the structure shape it resembles a worm. So it is known as vermiform appendix.
What is appendicitis?
Now let’s talk about what is appendicitis? As the name suggests appendicitis is basically inflammation of the appendix.
Appendicitis is inflammation of the appendix that can result in complications such as bowel perforation and peritonitis. The treatment modality of appendicitis is Appendectomy.
What are the causes of inflammation of the appendix?
- Obstruction
- Parasitic, bacterial, or viral infection
- Inflammatory bowel disease
- Tumours or growth
- Trauma

Obstruction – The most common cause of inflammation to the appendix is obstruction. let’s take a look at the appendix resembles somewhat is this. We know that whatever food comes into the large intestine a certain amount of undigested food or let’s say some seeds enter into the appendix that also goes out of the appendix. So it’s kind of a tube and that tube is open. But if there is an obstruction, obstruction most frequently is a fecalith. Fecalith is basically a hardened stool, a very hard stool that gets into the appendix but cannot move out of the appendix. If that happens, then obviously you know that there is an obstruction. So obstruction is the most common cause of appendicitis. Obstruction can be because of a fecalith, it can be because of some seeds, and it can be because of certain undigested food that is entered inside.
Parasitic or bacterial or viral infection – Another cause of appendicitis is some kind of parasitic or bacterial or viral infection. If we talk of parasitic infection, especially pinworm infection. Pinworm infection can cause appendicitis.
Inflammatory bowel disease – Another cause is inflammatory bowel disease. We know that an inflammatory bowel disease, inflammation of the Bowel, basically to the gastrointestinal system, and since the appendix is part of the system that can be inflammation to the appendix as well.
Tumours or growth – And also it could be because of certain tumours or growth. It can be some tumour that’s coming in and causing obstruction to the appendix, to the opening of the appendix basically. So tumours or any kind of growth can lead to appendicitis.
Trauma – Also, trauma can lead to appendicitis. So these are some of the risk factors or these are some of the causes of appendicitis.
Pathophysiology of appendicitis – Appendicitis symptoms
Now let’s talk about the pathophysiology of appendicitis or what happens in appendicitis.

As we have already discussed and we rooted the causes the major cause of appendicitis is obviously obstruction. An obstruction can be in the form of a faecolith or as undigested food or seeds or it could be because of a growth of tumour viral bacterial or parasitic infection. Now assuming that this is the obstruction.
What happens when there is obstruction?
When there is obstruction there is mucus secretion. Inside the lumen, there is mucus secretion. When there is a lot of mucus secretion we know that is going to be pressure, which’s going to increase the pressure. This is going to lead to increased pressure within the appendix. So there is increased pressure within the appendix. We also know that there are certain nerves innovating for the appendix. When there is pressure on these visceral nerves that going to lead to pain, nausea, and vomiting which are all signs and symptoms of clinical manifestations of appendicitis.
Migration of WBC due to bacteria
There is something else also happening. We know that there are few bacteria that is there inside the GI tract. So there are some bacteria inside the appendix as well. Now, this is not able to move out due to the obstruction. When these Bacteria is not able to move out because of the obstruction over here, it is going to multiply. Now the bacteria are multiplying due to which there is going to be inflammation, there is going to be a migration of WBC to this site. And now that is again going to cause an increase in pressure. With all that fluid accumulating, with all that inflammation happening inside the appendix, there is going to be a lot of pressure. That pressure is going to get transferred to the nerve. It is also going to get transferred to the blood vessel.
Ischemia and Gangrene
We’ve got blood vessels that are innovating this organ. So there is pressure on the blood vessels as well. If there is pressure on the blood vessels, that is going to lead to ischemia. It is going to block the blood vessels that are supplying the appendix which is going to lead to ischemia. It is going to lead to gangrene formation.
Now when this happens, these walls start to weaken gradually because of all that pressure because of all that inflammation and ischemia, gangrene the walls of the appendix gradually start becoming thinner and thinner. Now at one point in time, when this happens what is going to happen is this appendix is going to rupture. Now when that appendix ruptures what happens is whatever content was there inside is going to spill out. And where is it going to spill out? It’s going to spill out into the peritoneum which leads to peritonitis. So this is how an obstruction to the appendix leads to severe complications like peritonitis and bubble perforation. So that is about what happens in appendicitis.
Appendicitis assessment findings

Take a look at the assessment findings. The most important assessment finding is abdominal pain at McBurney’s point.
What is McBurney’s point?
McBurney’s point is basically a point from two-thirds the distance from the umbilicus to the right anterior superior iliac spine. Usually, the patient will complain of pain McBurney’s point.
There is rebound tenderness, there is a dominant rigidity, there is low-grade fever, elevated WBC count, anorexia nausea and vomiting, and there can be constipation or diarrhoea.
Why do all of these symptoms happen?
We have already discussed this when we talked about pathophysiology. You could also see that the patient assumes a side-lying position with abdominal guarding, that is knees flexed towards the chin and it’s kind of the patient is trying to guard his abdomen. So this happens on this particular feature because the patient is fine to get relief from pain. So you could see that the patient is in a lot of pain and the patient is assuming this position.
Ruptured appendix
We have already seen that the appendix can rupture and the appendix ruptures will lead to Bowel perforation and peritonitis. What are the signs and symptoms which should alert you if you have a patient who is having appendicitis?
What are the signs of a ruptured appendix?

What are the signs which should alert you if you have a patient having a ruptured appendix? The first one is guarding the abdomen. You will notice there is pallor because obviously all of those contents are building into the peritoneum. So the patient can go into shock, so might observe pallor. There is increased temperature and chills because there is a lot of bacteria as we saw earlier. And all these bacteria and infected material is thrown out into the peritoneum. There is restlessness, there is progressive abdominal distension, and abdominal pain. There are Tachycardia and Tachypnea.
What is appendicitis management?

The management is appendectomy or some people also called appendicectomy which is basically the removal of the appendix. So surgical removal of the appendix is a treatment for appendicitis.
Preoperative care – Appendectomy

Coming to preoperative care, now let’s assume that you have a patient who has a diagnosis of appendicitis and is posted for surgery. What is the care that you need to take in the pre-operative period?
Maintain NPO status – You need to maintain the NPO status. Provide IV fluids to prevent dehydration. Monitor for changes in the level of pain because if there is a lot of change in the level of pain or the severity of the pain is increasing it could indicate that there is perforation of the appendix, and rupture of the appendix. So you need to monitor for changes and levels of pain.
Monitor for signs of ruptured appendix and peritonitis – we have already discussed the signs, of tachycardia, tachypnea, abdominal guarding, tenderness, the rigidity of the abdomen, nausea, vomiting, restlessness, signs of hypovolemic shock all of these could be present if there is peritonitis or ruptured appendix.
Position in a right side-lying or low to semi-fowler’s position – Position in a right side-lying or low to semi-fowler’s position to promote comfort. So this will help in pain relief to a certain extent.
Monitor bowel sounds – If there is an accent bowel sound if there is a diminished bowel sound you need to alert the physician because that could mean that the appendix has ruptured.
Apply ice packs to the abdomen – Apply ice packs to the abdomen for 20 to 30 minutes every hour as prescribed. By applying ice packs so that there is some amount of pain relief as prescribed you have to apply the ice packs and it can be applied for around 20 to 30 minutes every hour.
Administer antibiotics as prescribed – To very very important things to remember when you are talking about a patient with appendicitis one is to avoid heat application and the second is to avoid laxatives or enemas. We don’t want to apply heat because heat may cause a rupture of the appendix because your appendix is already inflamed. Applying heat is going to lead to further vasodilation and that’s going to cause a rupture. This is why for an appendicitis patient we are applying a cold application and you need to avoid heat.
Laxatives and enemas – We know that when we give laxatives and enemas that is going to cause an increase in peristalsis. So if there is an increase in peristalsis then we know that the intestines are moving faster, other contents in the intestines are moving faster and that is a risk factor for rupture of the appendix. Because assuming that the large intestine and this is the appendix of the peristalsis is more there is more amount of stuff going to be travelling and going to cause more pressure into the appendix. That could ultimately lead to rupture.
Two very very important things to remember for a patient with appendicitis because both of these things can lead to rupture of the inflamed appendix:
- Avoid heat application
- Avoid giving laxatives or enemas

Postoperative care – Appendectomy
Postoperative care of appendectomy includes monitoring temperature for signs of infection, you need to monitor the insertion for all kinds of redness, swelling and pain, Keep the patient NPO until the bowel function has returned. Advance diet gradually as prescribed, so you will start with water and then slowly advance with a liquid diet and soft tide and foods according to the prescription of the dietitian. Administer antibiotics and analgesics. Maintain nasogastric (NG) suction and patency of the nasogastric tube if it is present. In some cases, an NG tube may be present. If it is present then you need to maintain the patency of the NG tube.
Postoperative care of a patient who has a ruptured appendix

There is a slight difference in the post-operative care of a patient who has a ruptured appendix during that there was rupture and it had caused peritonitis or the contents in the appendix had gone into the peritoneum. Then the post-operative care will differ slightly. Usually, what will happen if there will be a drain that will be present. So you will have to provide drain care. So there will be fused bleeding for the first 12 hours profuse not exactly bleeding they profuse discharge for the first 12 hours but after the first 12 hours, you should be able to see a gradual decline in the discharge that is coming out from the drain. Position the client on the right side-lying or low to semi-fowler’s position with legs flexed to facilitate the drainage. Dressing changes need to be done as per prescription. Record the amount and type of drainage. Perform wound irrigations if prescribed.
So that is about what happens in appendicitis and what is care for appendicitis.
A question for nurses
Look at one question and try to see whether we have understood the concept of appendicitis.
The question here:
The nurse is monitoring a client admitted to the hospital with the diagnosis of appendicitis who is scheduled for surgery in 2 hours. The client begins to complain of increased abdominal pain and begins to vomit. On assessment note that the abdomen is distended and bowel sounds are diminished. Which is the most appropriate nursing intervention?
Options
- Administer the prescribed pain medication
- Notify the Primary Health Care to provide
- Call and ask the operating room team to perform surgery as soon as possible
- Reposition the client and apply a heating pad on the warm setting to the client’s abdomen
Try to understand this question. Here we have a client who is admitted to the hospital with a diagnosis of appendicitis and you also know that this patient is scheduled for surgery in the next 2 hours. But all of a sudden the client starts to say that his abdominal pain has increased. So let’s mark that there is increased abdominal pain and the client also begins to vomit. When you assess you notice that the abdomen is distended and also see that the bowel sounds are diminished.
The question is asking which is the most appropriate nursing intervention. So your strategic keyword over here is the most appropriate nursing intervention. Now let’s take a look at these options.
The first option is to administer the prescribed pain medication. Administering the prescribed pain medication in this situation is not really the most appropriate. So we are going to eliminate that option because that is not the most important, the most appropriate thing to do at this point in time.
The second one says to notify the Primary Health Care provider. Now, look at the symptoms very carefully. The symptoms are indicating a complication. The symptoms say that there is increased abdominal pain, it says that the patient is vomiting, it says that the abdomen is distended and the bowel sounds are diminished. This means that our appendicitis patient’s appendix has ruptured. So here we’re looking at a patient who got a ruptured appendix. So the most appropriate thing to do is to notify the health care provider.
Let’s look at the third option. Call and ask the operating room team to perform surgery as soon as possible. The surgery is scheduled in 2 hours but it is not within the scope of nursing practice to call the operating room and ask the surgery team to do the surgery immediately. That decision has to be taken by the treating physician or the Primary Health Care provider. That is why this is not the most appropriate action to be done.
The fourth option is to reposition the client and apply a heating pad on the warm setting to the client’s abdomen. We’ve already seen first of all when there is an inflamed appendix you don’t use heat it and here looking at symptoms where we can say that the appendix has ruptured. So this is absolutely not to be done.
We can conclude that the most appropriate thing to do for this patient in this circumstance is to notify the Primary Health Care provider.
Conclusion
That is it about appendicitis. I hope that you have understood what is appendicitis, what appendicitis symptoms are, and the concept of appendicitis that we have discussed. The links below will help to get the references from where you can read more about appendicitis and its management. This article and video are mainly focused on the preparatory course for nurses who are planning to give their licensing exam for HAAD, MOH, DHA, Prometric, and NCLEX RN.
Thank you for the visit. Hope you enjoyed your reading.
Kindly share this article on your network and help others to read it.
Please leave your views about this article in the comments box and don’t forget to subscribe to this site.
Recommended for further reading:
- 10 Must Know Facts About Hand Sanitisers During COVID-19
- Primary Hyperaldosteronism | Causes And Nursing Management
- Regular Physical Activity – WHO Guidelines And Recommendations
For further reference: https://www.emedicine.medscape.com/article/773895-overview
References: YouTube Rinta Rajan

Mathukutty P. V. is the founder of Simply Life Tips. He is a Blogger, Content Writer, Influencer, and YouTuber. He is passionate about learning new skills. He is the Director of PokketCFO.
He lives with the notion of “SIMPLE LIVING, CREATIVE THINKING”. He Believes – “Sharing is caring.” and “Learning never ends.”





